What is egg collection?
Egg collection (also referred to as ‘egg retrieval’ or ‘egg pickup’) is the process by which we collect eggs from your ovaries. The eggs collected can then be frozen and stored, or used in the next step of an IVF cycle. Usually, we will be able to collect around 8–12 eggs but this is dependent on multiple factors, including your age.
Sometimes, you may need to undergo more than one egg collection, so we have a good quantity of eggs available (in the double digits is ideal). The number of eggs is important, whether you are freezing your eggs for potential use in later life, or whether you are moving on to the next step in the IVF process straightaway.
How do I prepare for my egg collection?
Two weeks before your egg collection
You will require regular hormone injections for around 8–14 days before your egg retrieval. This varies based on how your body is responding to the fertility medications and which regimen your fertility specialist decides is best for you. These injections encourage the maturation of eggs that would otherwise deteriorate. This is important as only mature eggs are capable of fertilisation when combined with sperm (an egg and sperm must successfully unite in order for an embryo to form).
While injections can sound painful and daunting, the needles are very small and easy to use. We will teach you (or a partner or another preferred person) how to give the injections at home.
You can read more about how we stimulate the ovaries to produce mature eggs.
The week prior to egg collection
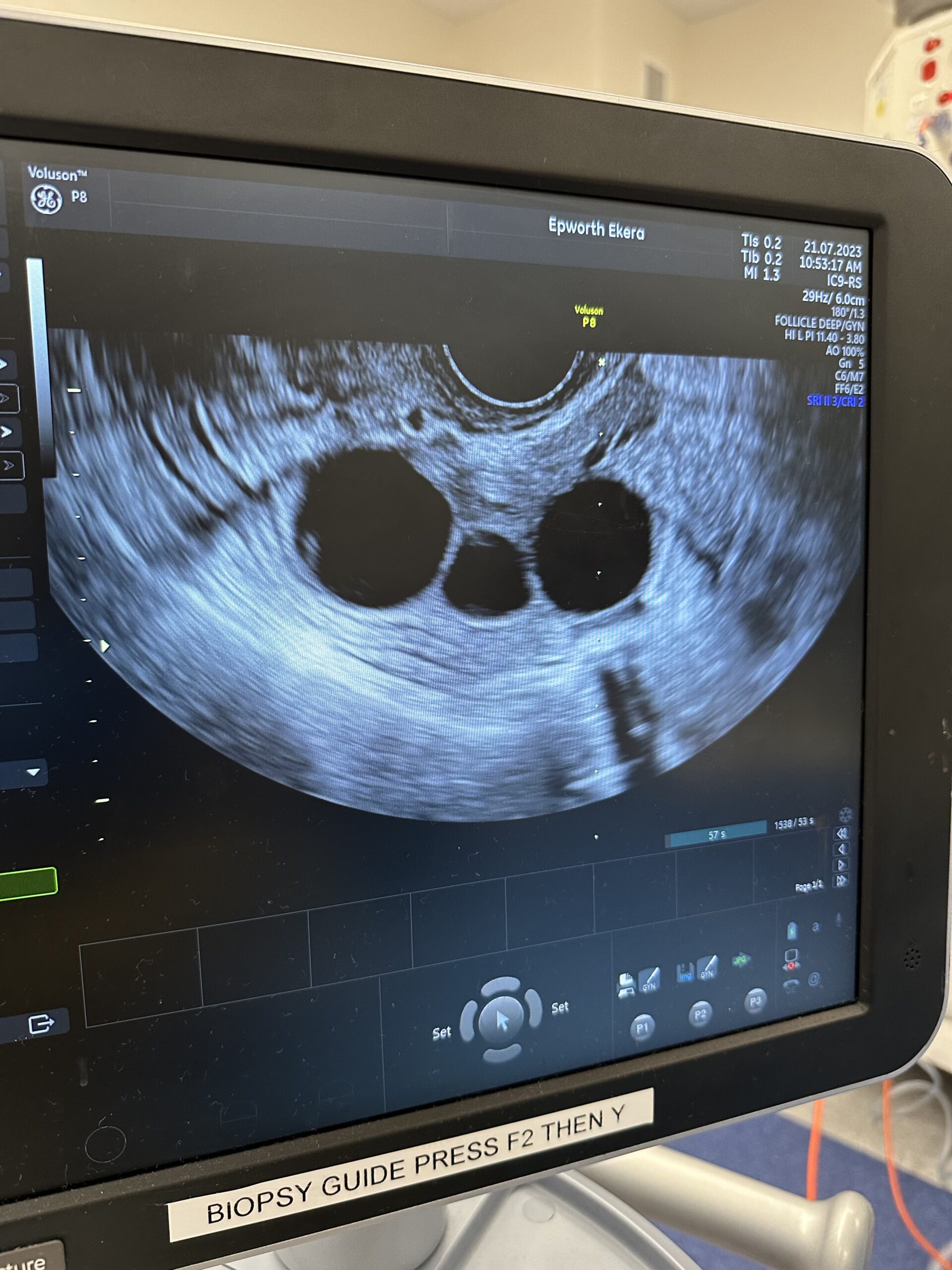
About a week after you start these medications, you will have a vaginal ultrasound so we can view your ovaries and count the number of follicles present. Usually, each follicle will contain one egg. The number of follicles gives us a good idea of how well you are responding to the fertility medications, while the size of the follicles is a good indicator of egg maturity. Unfortunately, small follicles usually contain immature eggs, which can be difficult to retrieve – they tend to stick to the follicle wall during collection. Thus, we may need to adjust your fertility medications to encourage more growth.
Ultrasound and blood tests also help us to determine the best time to collect your eggs. As such, these tests will be performed over the course of this week with the exact timing of your egg collection updated in line with your results. This change in schedule can sometimes be frustrating for patients, particularly in the midst of work commitments, but it ensures we are collecting your eggs at the optimal time in terms of both egg quantity and quality – the more mature eggs, the better!
1–2 days before your egg collection
Around 35–36 hours before your scheduled egg collection, you will have a ‘trigger injection’. This is a different hormone medication and will trigger ovulation (the release of eggs from your ovaries).
We will also ask you to fast from 6 hours before the time of your scheduled procedure (this reduces the risk of nausea and vomiting later).
Morning of your egg collection
On the morning of your egg collection, you may feel both excited and nervous – and hungry (!) from fasting. There are just a few things we need you to remember:
- Continue to eat and drink nothing. Small sips of clear fluids are okay up to 2 hours before your procedure
- Brush your teeth – we understand the last thing you want to do is to break our ‘nothing to drink’ rule but it’s okay to brush your teeth!
- Wear loose fitting, comfortable clothing
- Do not wear any makeup or jewellery, and
- Confirm the availability of the person you have organised to drive you home after your procedure and to ideally spend the rest of the day with you while your sedation wears off.
What will happen when I arrive for my egg collection?
On arrival, please make your way to our Ground Floor reception to complete your admissions paperwork. We will then guide you through to a waiting area where you can change into a hospital gown. There will usually be a period of waiting at this point, as we schedule your admission time an hour before your procedure. We recommend bringing a good book or podcast along.
Next, we will discuss the procedure with you, check when you took your trigger injection, answer any last-minute questions you may have, and ensure you understand and feel comfortable with what will happen next.
When it’s time for your procedure, we will guide you through to the procedure room and give you some light sedation. Once the sedation has kicked in (you will feel drowsy and relaxed), we will insert an ultrasound probe into your vagina. This provides a clear view of your ovaries and the follicles inside them (the eggs are located inside these follicles). We will then guide a fine needle attached to the probe into each of the follicles, one at a time. A suction device attached to the needle drives the fluid inside the follicle up the needle and into a heated test tube. This entire process takes around 20–30 minutes.
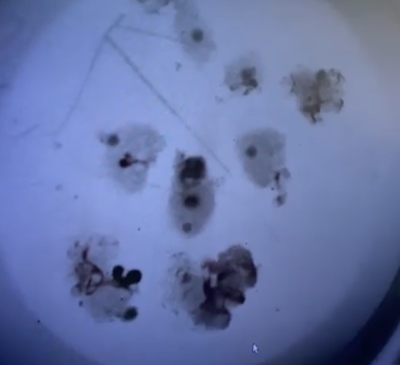
The fluid collected is taken straight through to our lab for examination by one of our embryologists. Under a microscope, they can carefully identify the eggs and discard the fluid. Our lab is directly adjacent to our day surgery so your eggs don’t have very far to travel!
If your egg collection is for the purposes of egg freezing, any mature eggs we find will be frozen and stored within a few hours of your procedure. If your egg collection is part of an IVF cycle, we may also freeze the mature eggs for use at a later date. Alternatively, we may proceed to the next step of the IVF process straightaway, placing your eggs with specially-prepared sperm from your partner or donor (this is called ‘insemination’).
Depending on how many eggs were collected and the volume of sperm available, 1–2 eggs will each be placed in a petri dish with a concentrated sperm sample containing around 100,000 sperm! Ideally, each egg will be fertilised by a single sperm, with every normally fertilised egg having the potential to grow and develop further into an embryo. However, it’s important to note that not every egg we collect will be mature, and not every mature egg placed with sperm will be fertilised. Hence, by collecting multiple eggs, we increase the chances of success at this step in the IVF process. You can read more about fertilisation and what impacts its success.
What happens after my egg retrieval?
Around 90 minutes after your procedure, your designated person can take you home. Before you leave, let us know if you need a medical certificate. We recommend taking it easy for the rest of the day.
If you are planning to freeze your eggs, we will generally call you later that day to tell you how many mature eggs were collected. If we are proceeding with insemination, we will usually call you the next day instead, so we can also tell you how many of these eggs were successfully fertilised overnight. Any fertilised eggs will be placed in an incubator in our lab. Here, their development will be monitored closely with the hope that they continue to grow into healthy embryos, ready for the next step in the IVF process – embryo transfer.
How can I best support my recovery after an egg collection?
Most women will experience some mild pain or discomfort after an egg collection and it may take weeks for this discomfort to ease completely. To help support your recovery, we recommend:
- Placing a heat pack over your belly and resting if you’re experiencing any cramping or discomfort. If your pain continues, take some paracetamol. Note: do not take any antihistamines, ibuprofen, aspirin or non-steroidal anti-inflammatory medications if you are planning to have an embryo transfer
- Consuming clear fluids if you are nauseous until you feel better
- Looking out for any vaginal bleeding (but don’t worry if you notice some light spotting or bleeding for a few days – this is completely normal)
- Avoiding vaginal creams, lubricants or spermicides (aside from the progesterone cream we may have given you)
- Avoiding all heavy lifting or vigorous exercise such as running or cycling for a few weeks
- Staying away from hot tubs and Jacuzzis
- Limiting your caffeine and alcohol intake
- Avoiding intercourse for a few days or until you feel comfortable. Engaging in intercourse around this time can result in natural conception; however, it’s important to listen to your body and only do what it feels physically ready for.
Are there any symptoms I should watch out for?
There are a few symptoms to watch out for after this procedure, including fever; pain, nausea or vomiting that’s not improving; heavy vaginal bleeding; feeling overly weak, faint or dizzy; shortness of breath; pain in your shoulder area; severe stomach bloating; rapid weight gain; or little to no urination despite drinking plenty of water.
If you are concerned or worried about anything you are experiencing, please call our clinic for advice on (03) 8080 8933. Alternatively, you can contact your fertility specialist. After-hours, you should visit your closest emergency department.
Still got questions?
If you have an upcoming egg collection booked and still have questions, don’t hesitate to give us a call on (03) 8080 8933. If you’re interested in learning more about egg freezing or IVF, check out the rest of our website for further information. For personalised advice, you can also book an appointment with one of our fertility specialists.